WHAT IS BREAST CANCER?
WHAT IS BREAST CANCER?
Breast cancer has become a major health problem in the last 50 years, affecting as many as one in eight women have during their lifetime. It has become a major health concern and is putting heavy financial burden on both developing and developed countries. In the family it affects, it causes immeasurable anxiety, suffering and loss. Hence, it is high time to implement an effective counter measure directed towards prevention, early diagnosis and an effective treatment.
Fig1: Structure of the breast:
TOP:
A = Milk duct B = Milk glan C = Enlarged portion of the duct
D = Openings on Nipple E = Fat
F = Muscle G = Rib
BOTTOM:
A = Duct cell B = Basement membrane C = Lumen
Risk Factors:
No single factor has been identified, as the cause of Breast Cancer while several predisposing factors could be the probable cause. They are grouped as genetic andfamilial factors, hormonal factors, dietary factors, benign breast diseases and environmental factors. Approximately half of all women who develop breast cancer have no identifiable risk factors.
- Sex: Though breast cancer is also seen in man, it is common in woman.
- Age: It is less common in the younger age. As age advances, chances of getting
breast cancer also increases.
- Genetic and family factors: A family history of breast cancer has been recognised as a risk factor for the disease. After gender and age, a positive family history is the strongest known predictive risk for breast cancer. It is known that in some of the “cancer families” there are specific mutations in single cancer susceptible genes. BRCA1 and BRCA2 are the two important genes whose presence increases the chances of getting breast cancer. The presence of Oncogenes like HER-2 also increases the risk. - Hormonal factors: Breast cancer is clearly related to hormone levels. An early menarche and late Menopause increases the chances, as does a late first pregnancy. The total duration of the menstrual life is an important risk factor for Breast cancer risk-the less the better.
- Diet: An increase in dietary fat intake is associated with increased incidence of the disease.
- Smoking & Alcohol: Multiple studies have shown an indication between alcohol consumption, smoking and risk of breast cancer.
- Benign breast lesion: They are classified as prolifierative, non-proliferative and atypical hyperplasia. Atypical hyperplasia is associated with an increase in risk of Cancer development.
- Environmental factors: As with many other cancers, exposure to certain environmental factors, such as Ionising radiation, electromagnetic fields and organo- chlorine pesticides increases the risk of Breast cancer.
Malignant tumours:
Malignant tumours can arise from any of the breast structures. Ductal carcinomas are the most common (78%), which arises from the milk ducts followed by lobular carcinoma (9%), which arises from the lobules, the milk secreting units of Breasts. These two cancers are aggressive and are known as Invasive Carcinomas. Other varieties are comparatively rare.
Investigations:
In 75% of cancers, the presenting symptom is a breast lump, most frequently in the upper outer quadrant of the Breast. However, the presence of a breast lump does not always indicate cancer. The majority of breast lumps (>90%) are benign. The commonest benign lumps are Cysts, fibro adenomas or areas of fibroadenosis.
The other common presenting symptoms are Breast pain and tenderness, change in Breast shape or size, dimpling, flaking or thickening of the skin of the breast, nipple inversion, rash or discharge and swelling of the upper arm or in arm pit.
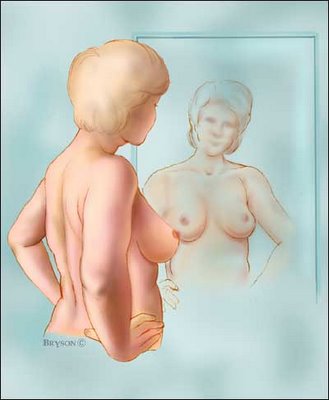
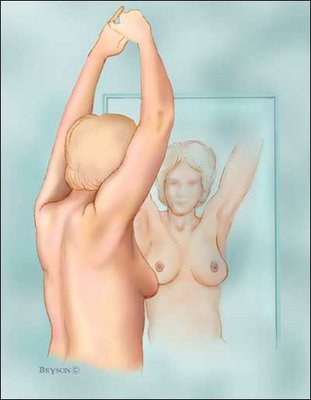
The three important methods to detect breast cancer early are Breast self-examination, Mammography and examination by qualified Oncologist.
All women aged more than 20 years, should perform monthly Breast self-examination on the 4th day of every menstrual cycle and are very useful in detecting the lump early. During examination, special attention should be paid to the above-mentioned presenting features. Women, who are under menopausal period, may perform the same, say on every 1st day of the month.
Mammography is special kind of X-ray examination of the breast. It can detect cases long before they become apparent by physical examination. Combined with clinical examination, it can be at least 90% accurate in its diagnosis. The following recommendation may be followed for Mammography.
- 40-49 years: Once in two years.
- >50 years: Once a year
- With a positive family history: Once a year after 35 years.
It is advisable to get the breast examined by qualified oncologist periodically as follows:
- 20-39 years: Once in every 3 years.
- >40 years: Once a year.
- With a positive family history: every year from 20th year onwards.
Diagnosis:
The diagnosis is always confirmed by either Fine needle aspiration Cytology (FNAC) or Open Biopsy. A needle is inserted in the lump and its cells are aspirated which are studied under the microscope. If the diagnosis is still in doubt, then an open biopsy or excision biopsy is done where the tumour is removed surgically and sent to the laboratory for a detailed study.
Staging:
The pre-treatment evaluation of a breast cancer patient should determine the clinical stage of the disease. There are four stages depending up on the location and spread of cancer.
Stage I: Breast alone
Stage II: Breast as for stage I and axillary nodes involved, but mobile
Stage III: Skin invaded, fixed or ulcerated, or tumour fixed to underlying muscle or pectoral fascia
Stage IV: Fixed axillary lymphadenopathy, supraclavicular involvement and/or distant metastases
A classification known as TNM (T=tumour, N=Node, M=Metastasis) classification is more useful and is used extensively where the size of the tumour, involvement of node and presence or absence of metastasis is taken in to account.
What Can Make Your Risk for Breast Cancer Go Down?
Eating a healthy diet
Losing extra weight
Regular exercise
Reducing alcohol use
Quitting smoking
Minimizing/eliminating extra estrogens
Preventive measures for high risk (surgery, medication)
What Can Make Your Risk for Breast Cancer Go Up?
Personal or family history
of breast cancer
Smoking
Excessive weight
Prolonged estrogens exposure
Abnormal breast cell growth
First full-term pregnancy after age 30
Never having a full-term pregnancy
Heavy alcohol use
Early start of menstruation
Late menopause
Factors affecting Breast Cancer
- Dr.N.Someswara