Health is Wealth. Health is a rare commodity. You can not buy it. No money can buy you good health. Hence you have to maintain your health.
One way of maintaining your health is to undergo periodical medical check ups. You have to undergo a set of medical tests and examination so that you can identify the beginning of disease and eradicate it completely before it gets its foot-hold in your body. After evaluaating your medical records and your physical examination, your Doctor will suitably advise you to modify your life style so that you can avoid diseases and promote your wellbeing.
The following article gives you a birds eye view of various tests and medical examinations that you may have to undergo periodically at different age times. This is only a general guideline. Your Doctor is the best person to select appropriate tests required for you and your family. In the following article, I have not mentioned general tests like Hb%, routine blood counts, routine Urine tests and routine stool tests and others. These are manadatory tests for any general medical examination. Hence I have not included. I have emphasized more on special tests. Now Go ahead! Read!! Get benefit from the same. You may write to me for any clarification.

Recommended Screening Procedures
-Ages 18-29
Its never too early to start taking care of your body. In addition to not smoking, eating right, maintaining a healthy weight, and exercising, following the screening recommendations on this chart can help you enjoy a healthy future.
1. Dental exam-Twice a year -To check for cavities and to have a cleaning, which may prevent gum disease
2. Eye exam-At least once between ages 20 and 39.
3. Skin exam-Every 3 years.
4. Skin self-examination-Monthly
- To look for changes, growths, or sores that don't heal. They should be reported to your Doctor.
- Here are the ABCD warning signs for marks on the skin :
- A is for Asymmetry, one half is unlike the other.
- B is for Border irregular, wavy, uneven border.
- C is for Color varied, different shades or colors
- D is for Diameter larger than a pencil eraser
- Protect your skin. Unprotected sun exposure over time can lead to skin cancer, including melanoma, a potentially deadly form of skin cancer. Melanoma is the most common form of cancer in women aged 25 to 29; so don't forget to reduce your exposure to the sun and to protect your skin with appropriate sun protection (SPF - 15 or greater) products when outside. Examine your skin on a monthly basis for any changes in appearance, including your legs, arms, abdomen, back, and face.
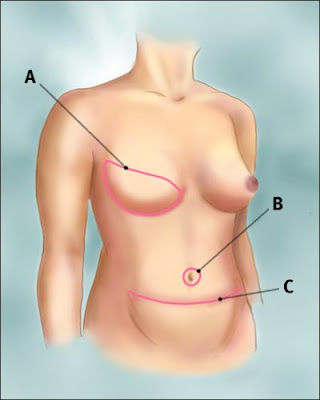
5. Clinical breast exam-Every 3 years.
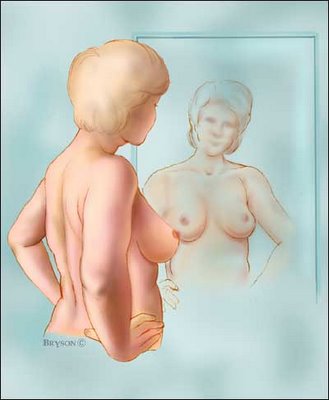
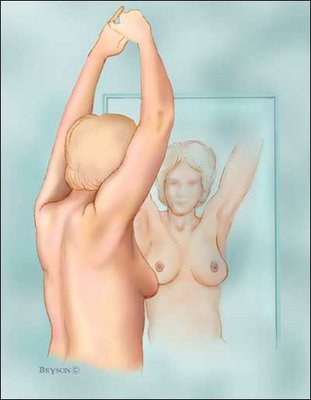
6. Breast self examination: Perform regular breast self-exams. Most breast lumps are found by women who check themselves during monthly breast self-exams. Ask your healthcare provider how to perform this important examination. Look and feel for changes in size, shape, contour, or skin texture. Call your healthcare provider if you notice any lumps or changes
7. Pap smear-Every year until 3 normal tests, then at a Doctor's discretion
Get a Pap test. You should start having Pap tests when you become sexually active or at age 18. Pap test screening, early identification and treatment can actually prevent the development of cervical cancer almost 100% of the time in younger women.
8. Pelvic exam-Every year.
Get advice about birth control and preconception care. The best time to prepare your body for a healthy pregnancy is long before you make a decision to become pregnant. This is called preconception care. Ask your doctor about a plan of action that is right for you. If you do not intend to become pregnant, ask your Doctor for advice on what form of birth control is best suited for you.
9. Sexually transmitted disease (STD) test(HIV, chlamydia, etc)-Whenever engaged in potentially risky behavior. Practice safe sex. Risky sexual behavior can include sex with new or multiple partners, inconsistent use of condoms, or unprotected sex with a partner who is not monogamous. Eighty-six percent of sexually transmitted diseases (STDs) eg, chlamydia, gonorrhea, genital warts, and HIV (the virus that causes AIDS) occur in people 15 to 29 years of age. HIV infection is among the top 10 causes of death in 15- to 24-year-olds. Always use a condom and get tested for STDs annually.
10. Cholesterol (total and HDL)-Every 5 years.
11. Blood pressure-At least every 2 years.
12. Immunizations: Tetanus boosters once in every 5 years. Get your immunizations. Protect yourself now by asking your healthcare provider about follow-up immunizations. Get vaccinated against hepatitis B, and make sure that you are up-to-date on your immunizations.
13. Osteoporosis prevention: Get enough calcium. Believe it or not, osteoporosis prevention begins now. So it's important to eat calcium-rich foods to build and preserve the strength and density of your bones. You need milligrams 1000 milligrams (mg) of calcium every day. You can achieve these levels by eating dairy products including non-fat, low-fat, and fortified. If you can't get enough calcium in to your diet, ask your Doctor to recommend a dietary supplement.
14. Chest-X-ray: PA View: There should be one base line chest x-ray of the chest. This functions as reference x-ray for your future chest problems. Just take one x-ray, at the age of 18 years! That is enough.
15. U/S pelvis & abdomen: A base line Ultra sound evaluation will give a lot of information about your internal structures like Liver, kidney, Uterus, Ovary and other organs. This should serve as a reference while your Doctoabdominal your abominal problems.
Recommended Screening Procedures -Ages 30-39
1. Dental exam-Twice a year: To check for cavities and to have a cleaning, which may prevent gum disease.
2. Eye exam-At least once between ages 20 and 39.
3. Skin exam-Every 3 years.
4. Skin self-exam-Monthly. To look for changes, growths, or sores that don't heal. They should be reported to your healthcare provider. Here are the ABCD warning signs for marks on the skin:
A is for Asymmetry-one half is unlike the other
B is for Border irregular-wavy, uneven border
C is for Color varied-different shades or colors
D is for Diameter-larger than a pencil eraser.
Protect your skin. Unprotected sun exposure over time can lead to skin cancer, including melanoma, a potentially deadly form of skin cancer. So reduce your exposure to the sun and protect your skin with appropriate sun protection (SPF >15) products when outside. Examine your skin on a monthly basis for any changes in appearance, including your legs, arms, abdomen, back, and face.
5. Clinical breast exam-Every 3 years.
6. Breast self-exam-Monthly. Most breast lumps are found by women who check themselves during monthly breast self-exams. Ask your healthcare provider how to perform this important examination. Look and feel for changes in size, shape, contour, or skin texture. Call your healthcare provider if you notice any lumps or changes.
7.Pap smear-Every year until 3 normal tests, then at a healthcare provider's discretion.
8. Pelvic exam-Every year: Get advice about birth control and preconception care. The best time to prepare your body for a healthy pregnancy is before you make a decision to become pregnant. This is called preconception care. Ask your Doctor, about a plan of action that is right for you. If you do not intend to become pregnant, ask your Doctor for advice on what form of birth control is best suited for you.
9. Sexually transmitted disease (STD) test(HIV, chlamydia etc): Whenever engaged in potentially risky behavior Practice safe sex. Risky sexual behavior can include sex with new or multiple partners, inconsistent use of condoms, or unprotected sex with a partner who may not be monogamous.
10. Cholesterol: Cholesterol (total and HDL)Click to learn more about understanding and controlling your levels. Every 5 years.
11. Blood pressure: At least every 2 years Check for high blood pressure, which can increase the risk of serious conditions like Stroke & Heart attack.
12. Immunizations: Get Tetanus boosters every 10 years.
13. Osteoporosis prevention: Get enough calcium. It's important to eat calcium-rich foods to build and preserve the strength and density of your bones. You need 1000 to 1500 milligrams (mg) of calcium every day. You can achieve these levels by eating dairy products including nonfat, low-fat, and fortified. If you can't get enough calcium into your diet, ask your Doctor to recommend a dietary supplement.
Recommended Screening Procedures -Ages 40-49
1. Dental exam-Twice a year. To check for cavities and to have a cleaning, which may prevent gum disease.
2.Eye exam-Every 2 years . To check vision and look for other conditions such as cataracts and glaucoma.
3. Skin exam-Every 3 years.
4. Skin self-exam-Monthly. To look for changes, growths, or sores that don't heal. They should be reported to your healthcare provider. Here are the ABCD warning signs for marks on the skin:
A is for Asymmetry-one half is unlike the other
B is for Border irregular-wavy, uneven border
C is for Color varied-different shades or colors
D is for Diameter-larger than a pencil eraser.
5. Mammogram-Every 1 to 2 years. To look for changes in the breast that can't be seen or felt. Start having regular mammograms. Why? Because breast cancer risk increases as you get older, starting at age 40. Women should have a mammogram and a clinical breast exam performed by a healthcare provider every 1 to 2 years. Early detection of breast cancer using mammograms may be lifesaving
6. Clinical breast exam-Every year.
7. Breast self-exam-Monthly. Most breast lumps are found by women who check themselves during monthly breast self-exams. Look and feel for changes in size, shape, contour, or skin texture. Call your Doctor, if you notice any lumps or changes.
8. Pelvic exam-Every year .
9. Pap smear- Every year until 3 normal tests, then at a Docotors discretion.
10. Sexually transmitted disease (STD) test(HIV, chlamydia, etc):
Whenever engaged in potentially risky behavior. Risky sexual behavior can include sex with new or multiple partners, inconsistent use of condoms, or unprotected sex with a partner who may not be monogamous.
11. Lipid profile: Once a year.
12. Blood pressure: At least once a year. High blood pressure affects your health. Check for high blood pressure, which can increase the risk of serious conditions like stroke and heart attack.
13. Diabetes screening: Once a year. Experts recommend that adults older than 40 be tested for adult onset diabetes, a condition in which blood sugar levels are too high. Millions have it and don't even know it because symptoms usually don't occur in the early stages. Obesity, or having excessive body fat, is a major risk factor for adult onset diabetes. Other risk factors include family history of adult onset diabetes, high cholesterol, high blood pressure, and a history of diabetes during pregnancy.
14: ECG in 12 leads: Once a year.
14. Immunizations: Get Tetanus booster opnce in every 5 years.
15. Osteoporosis prevention: Get enough calcium. It's important to eat calcium-rich foods to build and preserve the strength and density of your bones. You need 1000 to 1500 milligrams (mg) of calcium every day. You can achieve these levels by eating dairy products including nonfat, low-fat, and fortified. If you can't get enough calcium into your diet, ask your Doctor to recommend a dietary supplement.
16. Chest X-ray PA View: Just repeat another base line Chest X-ray at the begining of of your 40's.
17. U/S of Pelvis & abdomen: It is better to repeat once U/S of abdomen at the begining of your 40's.
Recommended Screening Procedures - over 50 years.
1. Dental exam-Twice a year. To check for cavities and to have a cleaning, which may prevent gum disease
2. Eye exam-Every 2 years . To check vision and look for other conditions such as cataracts and glaucoma.
3. Skin exam-Every year.
4. Skin self-exam-Monthly. To look for changes, growths, or sores that don't heal. They should be reported to your Doctor. Here are the ABCD warning signs for marks on the skin:
A is for Asymmetry-one half is unlike the other
B is for Border irregular-wavy, uneven border
C is for Color varied-different shades or colors
D is for Diameter-larger than a pencil eraser
5. Mammogram-Every year. Early detection and treatment of breast cancer may be lifesaving.
6. Clinical breast exam: Every year .To look for any changes and feel for any lumps.
7. Breast self-exam- Monthly. Most breast lumps are found by women who check themselves during monthly breast self-exams. Look and feel for changes in size, shape, contour, or skin texture. Call your healthcare provider if you notice any lumps or changes.
8. Pelvic exam- Every year.
9. Pap smear- Every year until 3 normal tests, then at a Doctor's discretion.
10. Sexually transmitted disease (STD) test(HIV, chlamydia, etc): Whenever engaged in potentially risky behavior. Risky sexual behavior can include sex with new or multiple partners, inconsistent use of condoms, or unprotected sex with a partner who may not be monogamous.
11.Lipid profile: Every year.
12. Blood pressure: Every year, One out of every 10 in their 50s have some degree or some type of heart disease. In Weman, when estrogen levels decrease, the risk of heart attack is similar to that for a man. Your Doctor can assess risk factors you may have, such as high blood pressure, high cholesterol, diabetes, and family history of heart diseases and develop an effective plan for good heart's health.
13. Diabetes screening: Once a year. Check for fasting and post prandial blood sugar levels.
14. Tread meal test (TMT): Once at the begining of 50th year which should serve as reference for future evaluations. Then depending up on your blood pressure, Diabetes, your weight, your physical activity, your stress level and family history, your Doctor will deside the frequency of this test.
15. Echocardiogram: Once at the begining of 50th year. This will serve as a baseline reference. It may repeated at the discretrion of your Doctor.
16. Immunizations: Get booster dose of Tetanus every 5 years. Pneumococcal vaccine once after age 65 and Influenza vaccine every year if 65 or older.
17. Fecal occult blood test- Every year. To test for blood in the stool, a possible sign of colon or rectal cancer.
18. Colorectal cancer tests (sigmoidoscopy, colonoscopy): This cancer is comparatively rare in Indians when compared to westerens. This may be done at the discretion of the Doctor once in every 5 to 10 years. Eating lots of fresh fruits, vegetables, and whole grains may reduce your risk of developing colon cancer.
19. Osteoporosis screening (bone mineral density test): As determined by your Docotr. It measures the density of your bones, can show if you have osteoporosis, and can predict your risk of spine and hip fractures. Your healthcare provider can discuss your risk factors with you and determine if you should have this test.
20. U/S of the pelvis & abdomen: This is done at the begining of the 50th year which will serve as a base line reference. Then this may be repeated every year at the discreation of your Doctor. This helps in early detection of BPH (Beningn Prostatic Hypertrophy)
21. Thyroid profile: Thyroid disease is common in women. An underactive thyroid (hypothyroidism) can cause fatigue, sensitivity to cold, weight gain, and other troubling symptoms. An overactive thyroid (hyperthyroidism) may cause rapid heartbeat, weight loss, and dizziness. A simple blood test done for thyroid-stimulating hormone (TSH) may detect a thyroid problem.
- Dr.N.Someswara